Sodium: Complete Guide
Sodium is an essential mineral that helps control fluid balance, nerve signaling, and muscle contraction. Most people get far more sodium than they need, largely from processed and restaurant foods, which can raise blood pressure and cardiovascular risk. This guide explains how sodium works, how much you likely need, when extra sodium is helpful (like heavy sweating), and how to balance sodium with potassium and overall diet quality.
What is Sodium?
Sodium is an essential dietary mineral and electrolyte (a charged particle in body fluids) that helps regulate fluid balance, blood pressure, nerve impulses, and muscle contraction. In foods, sodium is most commonly consumed as sodium chloride, which is table salt, but it also appears in many other compounds such as sodium bicarbonate (baking soda) and sodium-based preservatives.
Your body cannot make sodium, so you must get it from food and drink. At the same time, because sodium strongly influences how much water your body holds, the amount you consume and excrete has immediate effects on hydration status and longer-term effects on blood pressure for many people.
Two points help frame nearly every sodium discussion:
1. Sodium is necessary for life, but the amount required for basic physiology is relatively modest. 2. Modern diets often provide sodium in excess, mostly from packaged foods, sauces, breads, processed meats, and restaurant meals rather than from a salt shaker.
> Callout: Sodium is not inherently “bad.” The health impact depends on dose, your health status (especially blood pressure and kidney function), your potassium intake, and how much you sweat.
How Does Sodium Work?
Sodium’s effects come from its role as the major positively charged ion (cation) in extracellular fluid, meaning the fluid outside your cells. This positioning makes sodium a primary driver of water movement and blood volume.
Sodium, osmolality, and fluid balance
Your body tightly regulates the concentration of sodium in the blood (serum sodium), typically around 135 to 145 mmol/L. This concentration helps determine osmolality, which influences how water shifts between compartments (inside vs. outside cells).
When sodium concentration rises, the body triggers thirst and releases antidiuretic hormone (ADH) to retain water. When sodium concentration falls, the body suppresses ADH and increases water excretion. These adjustments help keep brain cells and other tissues from swelling or shrinking.
Blood pressure and the “volume” effect
Sodium increases extracellular fluid volume because water follows sodium. More volume can mean higher blood pressure, particularly in people who are salt-sensitive. Salt sensitivity is more common with aging, in people with hypertension, chronic kidney disease, diabetes, obesity, and in certain genetic backgrounds.
Blood pressure regulation is also influenced by:
- Kidney sodium handling (how much sodium is reabsorbed vs. excreted)
- Renin-angiotensin-aldosterone system (RAAS), which increases sodium retention when the body senses low effective blood volume
- Sympathetic nervous system activity
- Vascular function and stiffness, which often worsens with age
Nerve and muscle function
Sodium is critical for action potentials, the electrical signals that allow nerves to communicate and muscles to contract. Sodium flows into cells through ion channels, changing the electrical charge across cell membranes. This is foundational for:
- Skeletal muscle contraction
- Heart rhythm stability (in coordination with potassium, calcium, and magnesium)
- Digestive tract motility
The kidney’s central role
The kidneys are the main control system for sodium balance. They filter sodium from the blood and reabsorb most of it back into circulation, excreting the remainder in urine. Hormones like aldosterone increase sodium reabsorption, while natriuretic peptides promote sodium excretion.
This is why kidney health matters so much: when kidney function declines, sodium and fluid regulation becomes less flexible, increasing the risk of high blood pressure, swelling, and heart strain.
Benefits of Sodium
Sodium’s benefits are real, measurable, and immediate, especially when intake is too low for your needs or losses are high.
1) Maintains normal hydration and blood volume
Adequate sodium helps maintain plasma volume, which supports circulation, temperature regulation, and endurance capacity. If sodium intake is extremely low and fluid intake is high, serum sodium can drop, leading to symptoms ranging from fatigue and nausea to dangerous neurologic complications.
2) Supports nerve transmission and muscle contraction
Sodium is essential for neuromuscular function. Inadequate sodium, most often from excessive sweating combined with low intake, can contribute to:
- Muscle cramps or weakness
- Dizziness or lightheadedness
- Reduced exercise performance
3) Helps prevent hyponatremia in high-sweat contexts
Exercise-associated hyponatremia is usually driven by drinking large amounts of low-sodium fluids relative to sodium losses. For endurance athletes, military personnel, outdoor workers, and people exercising for hours in heat, sodium intake can be protective when paired with appropriate fluid strategy.
This connects to hydration misconceptions: plain water is often sufficient for typical daily activities, but for heavy sweaters or long-duration exercise, electrolyte balance matters, not just total fluid.
4) Enables effective oral rehydration
Sodium is a key ingredient in oral rehydration solutions (ORS) used for diarrhea, vomiting, or heat illness. Sodium improves water absorption in the gut via sodium-glucose co-transport, which is why ORS can rehydrate better than water alone in certain scenarios.
> Callout: Sodium can be performance-supportive and medically useful, but those benefits typically apply to specific situations (heavy sweat, gastrointestinal fluid loss, certain medications) rather than everyday overconsumption.
Potential Risks and Side Effects
For many people, the main concern is not sodium deficiency. It is chronic excess sodium intake coupled with low potassium intake and an overall ultra-processed diet.
1) Elevated blood pressure (hypertension)
High sodium intake is strongly linked to higher blood pressure at the population level. Even modest reductions in sodium can lower blood pressure, especially in salt-sensitive individuals. Because blood pressure is a major risk factor for stroke, heart attack, heart failure, and kidney disease, sodium reduction is a high-impact lever for many people.
People often underestimate sodium because it is hidden in:
- Bread and tortillas
- Soups and broths
- Sauces, dressings, and condiments
- Processed meats and cheese
- Fast food and restaurant meals
2) Increased cardiovascular risk
High sodium intake contributes to cardiovascular disease risk primarily through blood pressure, but may also relate to vascular stiffness and heart remodeling in susceptible individuals. For those with existing cardiovascular conditions, sodium can worsen fluid retention and symptoms.
3) Kidney strain and fluid retention
Excess sodium can increase fluid retention and raise blood pressure, both of which can accelerate kidney damage in vulnerable people. If you have chronic kidney disease, sodium restriction is often part of care to reduce swelling and blood pressure burden.
This ties into common kidney “sabotage” patterns: frequent ultra-processed meals, high blood pressure, dehydration, and certain medications can work together to impair kidney recovery.
4) Calcium loss and kidney stones (in some people)
Higher sodium intake increases urinary calcium excretion. In susceptible individuals, this may raise the risk of certain kidney stones and may be unfavorable for bone health if calcium intake is low. Adequate dietary calcium and moderation of sodium can help.
5) Hyponatremia from overhydration (a different sodium risk)
Low blood sodium (hyponatremia) is not usually from “not eating enough salt” day-to-day. It is more often from:
- Drinking excessive water during prolonged endurance activity
- Certain medications (notably thiazide diuretics, SSRIs in some cases)
- Medical conditions affecting water handling
6) Who should be especially cautious
You should be careful with sodium intake (and discuss targets with a clinician) if you have:
- Hypertension or strong family history of hypertension
- Heart failure or significant edema
- Chronic kidney disease
- Cirrhosis/ascites
- History of stroke
- Pregnancy-related hypertension
Practical Guide: How Much Sodium Do You Need and How to Get It Right?
Sodium guidance is often confusing because “optimal” depends on context. The goal is to avoid chronic excess for cardiometabolic health while ensuring enough sodium for normal function and sweat losses.
Daily intake targets (most adults)
Many major health organizations continue to recommend:
- Limit sodium to about 2,300 mg/day as a general upper target for adults.
- Aim closer to 1,500 mg/day for people with hypertension or higher cardiovascular risk, when feasible and clinically appropriate.
> Callout: If you do nothing else, reducing restaurant and ultra-processed foods is usually more effective than trying to “use less salt” at home.
When you may need more sodium
You may benefit from more sodium than average if you have high losses or special conditions, such as:
- Endurance exercise (especially longer than 90 minutes)
- Training or working in heat and humidity
- Very high sweat rate or salty sweat (white salt stains on clothing)
- Frequent sauna use combined with heavy sweating
- Gastrointestinal fluid loss (vomiting or diarrhea)
Sodium and hydration: what to do day-to-day
For typical daily life (desk work, short workouts), plain water and normal meals are usually enough. If you routinely feel lightheaded, crampy, or “washed out” after sweating, consider these steps:
1. Check the basics: Are you under-eating overall? Skipping meals? Over-consuming caffeine or alcohol? Sleeping poorly? 2. Add sodium strategically: Use a lightly salted meal, broth, or an electrolyte beverage around long/hot workouts. 3. Avoid overdrinking: Drink to thirst for most activities, and be cautious with forced high water intake.
This aligns with the broader hydration conversation: hydration is not only water, it is water plus electrolytes plus appropriate intake timing.
Best food sources and where sodium hides
Sodium occurs naturally in some foods, but the bulk comes from added sodium.
Higher-sodium foods (common sources):
- Pizza, sandwiches, burgers
- Deli meats, bacon, sausage
- Canned soups, instant noodles
- Sauces: soy sauce, teriyaki, ketchup, salad dressings
- Snack foods: chips, crackers
- Fast food and restaurant meals
- Fresh or frozen vegetables (without sauces)
- Fresh meats, poultry, fish (not cured or breaded)
- Beans cooked from dry (or no-salt-added canned, rinsed)
- Plain yogurt, milk
- Whole grains cooked without salty seasoning packets
Reading labels (quick method)
- Look at mg sodium per serving and the servings per container.
- As a simple rule, foods with 20% Daily Value (DV) or more per serving are considered high in sodium.
- Watch “stealth sodium” in breads, cereals, sauces, and condiments.
Practical strategies that work in real life
At home:
- Cook more often, use salt intentionally rather than relying on packaged seasoning blends.
- Use acid and aromatics to maintain flavor with less salt: lemon, vinegar, garlic, herbs, spices.
- Choose “no salt added” versions of broth, canned tomatoes, beans.
- Choose grilled or baked proteins over fried.
- Skip or reduce sauces, cheese, processed meats, and salty sides.
- Pick water or unsweetened drinks and avoid combo upgrades that add sodium and calories.
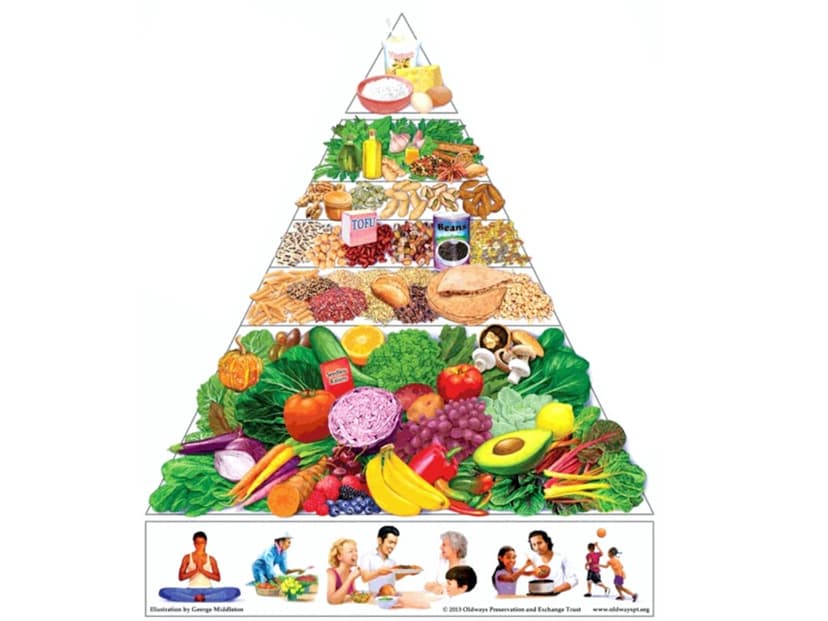
Sodium and potassium: the overlooked balance
Many sodium problems are also potassium problems. Diets high in fruits, vegetables, legumes, and dairy often provide more potassium, which can help lower blood pressure in many people (unless restricted for kidney disease).
Good potassium sources include:
- Beans and lentils
- Potatoes and sweet potatoes
- Leafy greens
- Yogurt
- Bananas, citrus, melons
What the Research Says
The sodium literature is large and sometimes contentious, mainly because measuring true sodium intake is difficult and because health effects vary by population.
Evidence we are confident about
1) Sodium reduction lowers blood pressure. Randomized feeding trials and controlled dietary interventions consistently show that lowering sodium reduces blood pressure. The effect is strongest in people with hypertension, older adults, and salt-sensitive individuals, but it is seen across many groups.
2) High blood pressure increases cardiovascular and kidney risk. The relationship between blood pressure and stroke, heart disease, heart failure, and kidney outcomes is among the most robust findings in public health.
3) Most sodium comes from processed and restaurant foods. Population studies repeatedly find that the majority of sodium intake is not from home cooking salt alone. This matters because sodium reduction often requires changing food patterns, not just a salt shaker.
Areas with nuance and ongoing debate
1) The “ideal” sodium target for everyone is not settled. Some observational studies have suggested a J-shaped curve, where very low reported sodium intake is associated with higher risk. However, these findings are heavily influenced by measurement error (spot urine estimates, reverse causality where sicker people eat less or restrict sodium) and confounding.
Most expert consensus still supports reducing high sodium intakes, particularly in populations with prevalent hypertension and low potassium intake.
2) Individual variability is real. Salt sensitivity varies. Genetics, kidney function, insulin resistance, age, and overall diet quality influence how strongly sodium affects blood pressure.
3) Athletes are a special case. Sports nutrition research supports sodium replacement during prolonged exercise, especially in heat, to help maintain performance and reduce hyponatremia risk. But outside endurance contexts, routine high sodium supplementation is not supported.
What matters as much as sodium
Research increasingly emphasizes dietary patterns: diets like DASH-style eating (more fruits, vegetables, legumes, low-fat dairy, less ultra-processed food) improve blood pressure through multiple mechanisms, including higher potassium, magnesium, fiber, and lower sodium.Who Should Consider Sodium (and What That Means)
Because sodium is essential, everyone “needs” it. The more practical question is who should prioritize limiting sodium vs. who should plan for replacement.
People who should prioritize lowering sodium
- Anyone with high blood pressure or borderline readings
- Adults over 50, as salt sensitivity increases with age
- People with chronic kidney disease or a history of kidney decline
- People with heart failure or frequent swelling
- People with diabetes or metabolic syndrome, who often have higher cardiovascular risk
People who may need intentional sodium replacement
- Endurance athletes (running, cycling, triathlon)
- Outdoor workers, military, firefighters
- Individuals with frequent long sauna sessions plus heavy sweating
- People with acute gastrointestinal illness (use oral rehydration strategies)
People who need individualized medical guidance
- Chronic kidney disease (sodium and potassium targets may both be individualized)
- Heart failure (fluid and sodium often coordinated)
- People on diuretics or other medications affecting electrolytes
- People with a history of hyponatremia
Common Mistakes, Interactions, and Related Conditions
Common mistakes
Mistake 1: Focusing only on table salt. Most sodium comes from packaged and restaurant foods. If you cook mostly at home, you can often use small amounts of salt and still land lower than average.
Mistake 2: Replacing salt with sugar or ultra-processed “low-sodium” foods. Some products reduce sodium but increase added sugars or additives. The bigger win is choosing minimally processed foods.
Mistake 3: Overhydrating with plain water during long exercise. This can dilute blood sodium and raise hyponatremia risk. Match fluids to thirst and include sodium for long, sweaty sessions.
Mistake 4: Assuming symptoms equal “low sodium.” Fatigue, headaches, cramps, and dizziness have many causes. If symptoms are persistent or severe, evaluate blood pressure, iron status, sleep, fueling, and medications.
Medication and supplement interactions
- Diuretics: Can increase sodium loss (some types) and alter potassium balance. Sodium targets may need adjustment.
- ACE inhibitors/ARBs: Often used for blood pressure and kidney protection; may raise potassium, which changes the sodium-potassium balance conversation.
- NSAIDs: Can promote fluid retention and raise blood pressure in some people, making high sodium intake more problematic.
- Electrolyte supplements: Useful for heavy sweating, but can add large sodium doses quickly. Track total intake if you have hypertension.
Related conditions where sodium often comes up
- Hypertension: Sodium reduction plus potassium-rich foods often improves readings.
- Kidney disease: Sodium restriction commonly recommended to reduce BP and swelling.
- Heart failure: Sodium and fluid management can reduce symptoms.
- Kidney stones: Lowering sodium may reduce urinary calcium; hydration and diet pattern matter.
- Inflammation and ultra-processed diets: High sodium frequently co-travels with ultra-processed foods that may worsen cardiometabolic markers; improving overall diet quality often reduces sodium automatically.
Frequently Asked Questions
Is sodium the same as salt?
Not exactly. Salt usually refers to sodium chloride. Sodium is the mineral component. Salt is about 40% sodium by weight, so 1 teaspoon of table salt (about 6 grams) provides roughly 2,300 mg sodium.How do I know if I eat too much sodium?
Common clues include frequent reliance on packaged foods or restaurant meals, and label totals that exceed 2,300 mg/day. The most meaningful health signal is blood pressure over time. Home blood pressure tracking can help you see whether sodium reduction improves your readings.Can I eat too little sodium?
Yes, but it is uncommon with typical diets. Risk is higher with prolonged heavy sweating, endurance events, or overhydration with plain water, and with certain medications. Severe low sodium is a medical issue.Are “sea salt” and “Himalayan salt” healthier?
They are nutritionally similar to table salt in terms of sodium content. Trace minerals in specialty salts are too small to meaningfully impact health. Iodized salt can be beneficial for iodine intake if you do not get iodine elsewhere.Do electrolyte drinks help with everyday hydration?
For most people doing normal daily activities or short workouts, water and regular meals are enough. Electrolytes can help during long, sweaty exercise, heat exposure, or gastrointestinal fluid loss. If you have hypertension, choose lower-sodium options unless you truly need replacement.What is the fastest way to lower sodium without feeling deprived?
Reduce the biggest contributors first: restaurant meals, processed meats, salty sauces, and packaged snacks. Replace with simple meals built around whole proteins, vegetables, beans, fruit, and minimally processed grains. Use herbs, spices, citrus, and vinegar to keep flavor high.Key Takeaways
- Sodium is an essential electrolyte that regulates fluid balance, nerve signaling, and muscle function.
- Most people consume more sodium than needed, mainly from processed and restaurant foods, not the salt shaker.
- Chronic high sodium intake can raise blood pressure and increase cardiovascular and kidney risk, especially in salt-sensitive individuals.
- Sodium can be beneficial in specific contexts like prolonged sweating, heat exposure, endurance exercise, and oral rehydration.
- Practical improvement usually comes from changing food patterns: fewer ultra-processed foods, more whole foods, and better sodium-potassium balance.
- If you have hypertension, kidney disease, heart failure, or take certain medications, sodium targets should be individualized with clinical guidance.
Glossary Definition
Sodium is a mineral that helps regulate fluids and is found in table salt and many foods.
View full glossary entryHave questions about Sodium: Complete Guide?
Ask Clara, our AI health assistant, for personalized answers based on evidence-based research.