What Really Changes When You Quit Sugar for 30 Days
Summary
Quitting sugar for 30 days is framed here as a nervous system and reward-system reset, not a willpower contest. The first 1 to 2 days can feel like withdrawal, including irritability, headaches, and feeling flat, but early liver benefits may start quickly as fructose load drops. By days 3 to 7, cravings often loosen their grip, blood sugar swings may calm, and hunger hormones can start communicating more normally. Over weeks 2 to 4, taste buds “recalibrate,” sleep and mood may steady, and metabolic markers like triglycerides may improve. Results vary, especially with insulin resistance.
🎯 Key Takeaways
- ✓This 30-day approach frames sugar reduction as reward-system rehab, dopamine sensitivity can begin to normalize after the first few days.
- ✓Cutting added sugar sharply reduces fructose burden on the liver, which may lower de novo lipogenesis and triglycerides over time.
- ✓By about a week, hunger and satiety signaling (insulin, leptin, ghrelin) may feel more predictable, which can make appetite easier to manage.
- ✓Taste buds often reset, natural foods can taste sweeter, while highly sweet foods may start tasting “fake” or unpleasant.
- ✓The plan emphasizes environment design (remove sugar from the house, do not skip meals) over relying on willpower.
“Will I feel terrible if I quit sugar?” Start with the nervous system
A common question is, “If I quit sugar for 30 days, will I feel worse before I feel better?”
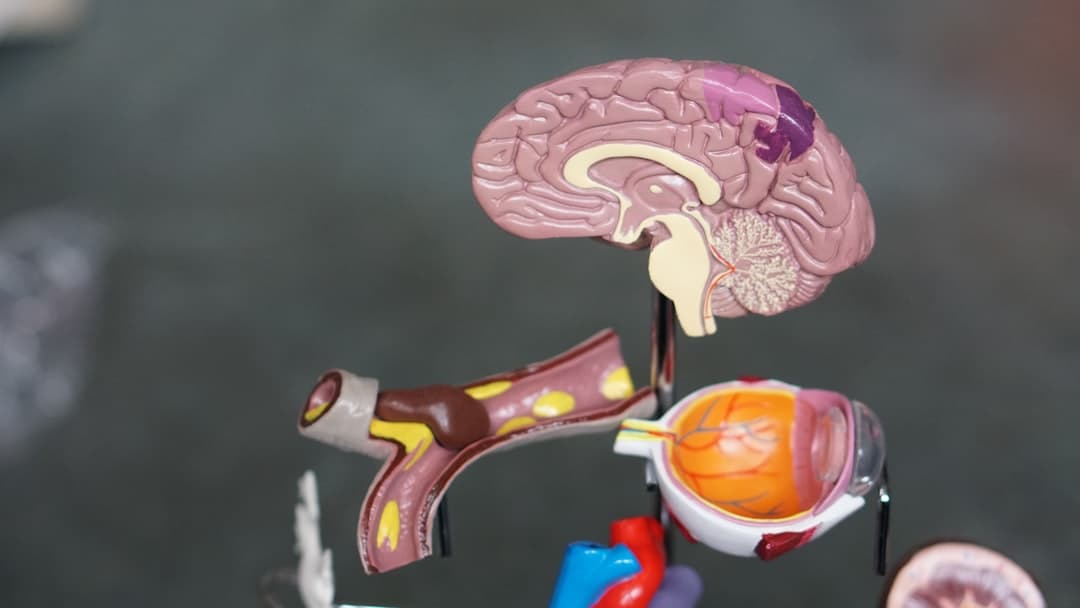
This day-by-day framework treats that early discomfort as a predictable nervous system response, not a personal failure. The core idea is that frequent sugar intake trains the brain to expect rapid, repeatable pleasure signals. When the signal disappears, the brain can react like something important is missing.
What makes this perspective different from a generic “eat less sugar” article is the emphasis on reward circuitry, especially dopamine, and on the idea that the first week is basically a recalibration phase. It is less about moralizing food choices and more about understanding the operating system you are working with.
Sugar is framed as “drug-like” because it can produce fast reward learning, the kind that makes you want the next hit. That does not mean sugar is identical to street drugs, but it does highlight a shared mechanism: repeated quick rewards can teach the brain to seek more stimulation.
Here is the hopeful part.
The timeline is designed to show that cravings and mood changes tend to shift in phases. If you can recognize the phase you are in, you can stop interpreting discomfort as “this is just who I am,” and start seeing it as “this is my brain recalibrating.”
Did you know? Many health organizations recommend limiting added sugars to reduce cardiometabolic risk. For example, the American Heart Association suggests a low daily limit for added sugars for many adults, because excess intake is linked with higher risk factors over time, including triglycerides and weight gain (American Heart Association added sugars guidanceTrusted Source).
Days 1 to 2: reward withdrawal, plus early liver relief
The first two days are positioned as the hardest for one reason: reward system withdrawal.
When sugar has been a frequent “finish the meal” ritual or a stress response, removing it can feel like you took away the brain’s easiest tool for comfort. The discussion centers on dopamine as the chemical that helps regulate desire, motivation, and reward. When the system is working well, dopamine supports curiosity and goal-oriented behavior. When the system is repeatedly flooded with fast rewards, the threshold can shift, normal life feels less satisfying, and the brain starts asking for stronger or sweeter hits.
That is why day 1 can feel like “panic.” Not because you are weak, but because your brain has been trained to expect a certain signal at certain times.
What you might notice on days 1 to 2
These early symptoms are described as common and temporary:
A key practical point is not to stack too many changes at once. The strategy is not “quit sugar and also skip meals and also start a punishing diet.” The idea is to keep the body calm while the reward system adjusts.
The liver angle, why fructose matters here
Alongside the nervous system story, there is a strong liver story.
This framing emphasizes how much sugar many people consume and how much of that becomes a fructose burden. Half of table sugar (sucrose) is fructose, and high fructose corn syrup is roughly similar. Fructose is handled largely by the liver, and the discussion compares heavy fructose load to alcohol in terms of liver processing burden. It is not saying fructose is literally alcohol, but it uses the comparison to make the point that the liver can be overworked.
The “early win” is that when you cut added sugar, the liver may immediately face far less fructose. That can reduce de novo lipogenesis (the process of making fat from non-fat sources) over time. In some people, triglycerides may begin to drop, although the timing can vary, especially if insulin resistance is significant.
What the research shows: High intake of added sugars, especially sugar-sweetened beverages, is associated with higher cardiometabolic risk markers in population studies. Guidance from the World Health Organization recommends reducing free sugars to support long-term health (WHO guideline on sugars intakeTrusted Source).
Important: If you have diabetes, take insulin or sulfonylureas, or have a history of disordered eating, changing carbohydrate patterns can affect appetite and blood sugar. It is safest to plan changes with a clinician who knows your medical history.
What to stop, and what to eat instead (without going extreme)
This approach is not presented as a strict ketogenic plan. The emphasis is “reasonable,” whole-food eating that removes the strongest sugar triggers.
It also makes a point that helps many people: cravings are not only internal, they are environmental. If sugar is in the house, your brain is going to keep getting cues.
Here is the “stop list” as described, with the logic behind it.
And here is the “eat list,” designed to keep you satisfied so you do not rebound.
A big misconception this challenges is the idea that success depends on iron will.
This perspective argues that brain chemistry drives behavior, so you “set the game up in your favor.” That means removing triggers, eating regular meals, and not negotiating with yourself at 9 pm in front of the pantry.
Pro Tip: Before day 1, do a 10-minute “friction audit.” Put sweets, sugary drinks, and dessert foods out of the house, or at least out of sight, so your brain gets fewer cues during the withdrawal window.
»MORE: If you want a simple companion tool, create a one-page “sugar swap list” for your kitchen. Write three go-to breakfasts, three lunches, three dinners, and three snack options that are protein-forward and low in added sugar.
Days 3 to 4: early adaptation, steadier energy, gut shifts begin
Days 3 and 4 are described as the start of early adaptation.
You are not “done,” but the intensity often changes. The idea is that dopamine receptors begin to re-sensitize, and natural food starts to feel more rewarding. This is also where many people notice fewer dramatic blood sugar swings after meals.
A subtle but important theme here is the difference between physiologic cravings and habitual cravings. Physiology may calm down first, while habits linger. You might still want something sweet at the time you always have it, like after dinner or during an afternoon break, even if your body is not truly demanding it.
What may be happening in the gut
By around day 3, the discussion suggests the gut microbiome can begin shifting away from “sugar-loving” bacteria. The concept is simple: if you stop feeding fast sugars, microbes that thrive on that fuel may decrease, and other microbes may gain ground.
Research increasingly supports that dietary patterns can shift the gut microbiome relatively quickly, although the exact timeline and outcomes vary by person, baseline diet, and fiber intake. Broadly, diets higher in whole plant foods and fiber can support microbial diversity and beneficial metabolites like short-chain fatty acids (NIH overview of the human microbiomeTrusted Source).
What you might notice on days 3 to 4
One of the most distinctive observations in this timeline is the “new sweetness” phenomenon.
As your threshold changes, you may start noticing subtle sweetness in foods you never considered sweet before. That shift can be motivating because it is evidence that your nervous system is adapting.
Days 5 to 7: hunger hormones start “talking” again
By days 5 to 7, the reward circuits are described as calming down.
This is where the discussion moves from dopamine into hunger hormones. The focus is on three signals: insulin, leptin, and ghrelin.
Insulin helps move nutrients from food into cells. Leptin is often described as a satiety signal, the “we are full” message. Ghrelin is a hunger signal that tends to rise when the body expects food. The argument is that when a diet is dominated by sugar and ultra-processed foods, these signals can become noisy and disconnected. When you remove added sugar, the signals may start coordinating again.
This matters because appetite can start matching energy needs more naturally. The comparison used is that animals generally eat until full and stop, while humans can override satiety when foods bypass normal regulation.
Sleep enters the picture here too.
With fewer blood sugar swings and less cortisol disruption, some people notice they wake less at night. It is not guaranteed, but it is a common report.
A small but practical physiological point is also included: reduced insulin pressure can lead the kidneys to retain less sodium, which can reduce water retention. Some people notice less puffiness, and blood pressure may drop a few points.
Expert Q&A
Q: Why do I crave dessert after dinner even when I am full?
A: For many people, that after-dinner dessert pull is a learned reward loop, not true hunger. Your brain pairs “meal finished” with “sweet reward,” so the cue can fire automatically.
In the first week, it can help to replace the ritual, for example herbal tea, a walk, or a crunchy, savory option, while your reward system recalibrates.
Health educator perspective based on nervous-system reward learning, not a diagnosis
Days 8 to 14: fewer cravings, calmer mood, inflammation trends
Days 8 to 10 continue the hormone rebalancing theme.
Ghrelin is described as becoming less random, aligning more with meal timing. Leptin sensitivity may improve, meaning you feel full sooner when you are supposed to. The gut story also continues, with an emphasis on bacteria that produce butyrate, a short-chain fatty acid often associated with gut barrier support.
Some people report clearer skin and less bloating around this time. Those are not guaranteed outcomes, but they are plausible for individuals who were reacting to high sugar intake, frequent ultra-processed foods, or large swings in insulin.
Days 11 to 14 add a more detailed liver-gut loop.
The discussion highlights reduced export of triglyceride-carrying particles (VLDL) as the liver makes less fat from fructose. It also mentions that liver enzymes like ALT may improve in some people if they were elevated due to liver stress. Better liver function can support bile flow, which supports fat digestion, which in turn can support gut function.
Inflammation markers are also mentioned, specifically interleukin-6 and tumor necrosis factor alpha, as examples of measurable signals that may decrease when overall metabolic stress decreases.
This is where it helps to separate two ideas that often get mixed up.
First, quitting sugar does not “detox” you in a magical way overnight. Second, reducing added sugar can reduce metabolic burden, and over time that may support healthier liver fat handling and inflammatory balance. The body already has detox systems, the change is reducing what overwhelms them.
What the research shows: Diets high in sugar-sweetened beverages are associated with increased risk of weight gain and type 2 diabetes in large observational research, and reducing these beverages is a common public health target (CDC overview on added sugarsTrusted Source).
A noticeable quality-of-life change often reported in this window is fewer afternoon slumps.
Instead of the classic mid-afternoon crash, energy can feel more even. People also commonly describe waking up less groggy.
Days 15 to 21: taste buds reset, triggers lose power, rhythm returns
By days 15 to 17, the reward system reset is described as deeper.
One practical marker is that external cues lose force. Someone can eat a cookie nearby and you may not feel that emotional surge of “I need that now.” This is a big deal because many people assume cravings are purely internal, when in reality they are often cue-driven.
Taste changes become more dramatic.
The sweetness threshold is described as higher, meaning fruit tastes intensely sweet on its own. Foods you used to “need” sugar on, like berries, may feel complete without toppings. In contrast, very sweet processed foods may start tasting fake or even nauseating.
Days 18 to 21 emphasize “metabolic rhythm” and cellular energy.
The discussion suggests there may be measurably less fat stored in the liver over time, and that mitochondria can work more efficiently with less oxidative stress. Mitochondria are described like engines that burn fuel with oxygen, producing inevitable “smoke.” The claim is that when the system is more efficient, there is less reactive oxygen species.
Sleep rhythm is also revisited.
As metabolism stabilizes, cortisol and melatonin rhythms may become more consistent, supporting deeper sleep and more alert mornings.
Then there is a key nervous system pairing: dopamine and serotonin.
Dopamine is framed as desire and quick reward seeking, while serotonin is framed as contentment and stability. The argument is that heavy reliance on sugar trains you toward “more, more, more,” while restoring balance supports “I am good, I have enough.” This is presented as a foundation for enjoying life without needing constant external hits.
A note on methylation and the MTHFR mention
The final part of this window introduces methylation and B vitamins as support for neurotransmitter recycling, liver metabolism, and inflammation control. It also mentions that many people have MTHFR variants and therefore may process certain B vitamins differently.
This is an area where nuance matters. Genetic variants like MTHFR are common, but the health impact varies widely, and supplementation decisions depend on lab results, diet, medications, and individual risks. If you are considering methylated B vitamins, it is reasonable to discuss it with a clinician, especially if you are pregnant, taking medications that interact with folate metabolism, or have a history of B12 deficiency.
Important: If you are considering supplements for mood, energy, or “detox,” ask a clinician about interactions and whether testing is appropriate. Supplements can be helpful for some people, but they are not risk-free.
Days 22 to 30: a new baseline, and why it can feel “worth it”
The final week is framed as a new metabolic baseline.
The claim is not just “you avoided sugar,” it is “you now enjoy food differently.” Pleasure comes more from the quality of the meal and how it is prepared, less from drug-like stimulation.
Metabolic markers are listed as areas that may improve over time, including fasting glucose, A1C, fasting insulin, triglycerides, and VLDL. The discussion also mentions LDL particle number and size as potentially improving with reduced inflammation and better metabolism, even if LDL cholesterol in mg/dL does not move the way people expect.
This is also where the video connects sugar reduction to long-term risk.
The argument is that improving these markers can reduce risk or incidence over time for cardiovascular disease, type 2 diabetes, high blood pressure, stroke, and dementia. Those outcomes are influenced by many factors, but reducing added sugar is a reasonable lever for many people, especially when it replaces ultra-processed foods with whole foods.
The day-to-day lived experience matters most to many people.
By this point, cravings are often described as gone or quiet. Appetite feels like it belongs to you again. Energy becomes more “all day” rather than spiky. Sleep, digestion, and mood may all feel steadier.
And there is one more psychological point that shapes this whole approach.
If you slip, the instruction is simple: start again. The goal is not perfection, it is repetition until the nervous system learns a new normal.
How to run your own 30-day sugar reset (simple, action-focused)
Clear the cues before day 1. Remove sweets, sugary drinks, and “dessert defaults” from your home or workspace. This reduces the number of decisions you have to win during withdrawal.
Do not skip meals in the first week. Build meals around protein, vegetables, and satisfying fats so you are not fighting hunger and withdrawal at the same time.
Plan a replacement ritual for your trigger time. If 9 pm is your sugar time, decide what happens instead, tea, a shower, a walk, a book, or a savory snack.
Expect cravings to be cue-based after day 3. When a craving hits, ask, “Is this hunger, habit, or emotion?” That one question often breaks the automatic loop.
Reintroduce sweetness thoughtfully after day 30. If you choose to bring back treats, do it intentionally, not as a reflex. Many people do better with planned portions than with “whenever.”
Expert Q&A
Q: Is fruit basically the same as sugar, and should I cut it out too?
A: This approach treats whole fruit differently than added sugars because fruit comes with fiber, water, and a slower eating pace. That said, if fruit becomes a trigger that keeps cravings alive, some people do better focusing on berries and seasonal fruit portions.
If you have diabetes or need carbohydrate targets, it is best to individualize fruit intake with a clinician or dietitian.
Nutrition education perspective, not medical advice
Key Takeaways
Frequently Asked Questions
- What symptoms are common in the first few days of quitting sugar?
- Many people notice irritability, headaches, fatigue, mental fog, and a “flat” mood in days 1 to 2. These are often described as short-term reward-system withdrawal effects that may ease as cravings become less physiologic and more habit-based.
- How long do sugar cravings usually last when you quit?
- In this day-by-day framework, cravings often loosen significantly by around day 3, and many people report they are much quieter by days 5 to 7. Habit triggers can still appear, especially at usual snack times or in social settings.
- Do I need to go keto to quit sugar for 30 days?
- No. The approach emphasizes whole foods, adequate protein, and satisfying fats, while allowing some slower-digesting grains and legumes if desired. The main target is added sugar and highly processed foods, not all carbohydrates.
- Is juice a good substitute when quitting sugar?
- Juice is still a concentrated sugar source and can deliver a fast sugar hit similar to other sweet drinks. If your goal is to reduce reward-loop stimulation and blood sugar swings, whole fruit is generally a more supportive option than juice.
- Can quitting sugar help sleep and mood?
- Some people report fewer nighttime awakenings and steadier mood after the first week, possibly related to fewer blood sugar swings and a calmer reward system. Results vary, and sleep and mood are influenced by many factors beyond diet.
Get Evidence-Based Health Tips
Join readers getting weekly insights on health, nutrition, and wellness. No spam, ever.
No spam. Unsubscribe anytime.