Uncomfortable Vaccine Questions, Explained Clearly
Summary
If you have ever looked at the childhood schedule, heard a scary claim from a credentialed person, or wondered how vaccines can be “safe” when rare side effects exist, this article is for you. Based on Dr. Paul Offit’s conversation, the core message is that vaccine decisions are made with the question “Do we know enough,” not “Do we know everything.” The discussion walks through how trials and real-world monitoring work together, why some risks only appear after millions of doses, and why clear communication matters as much as data.
The moment vaccine questions start to feel personal
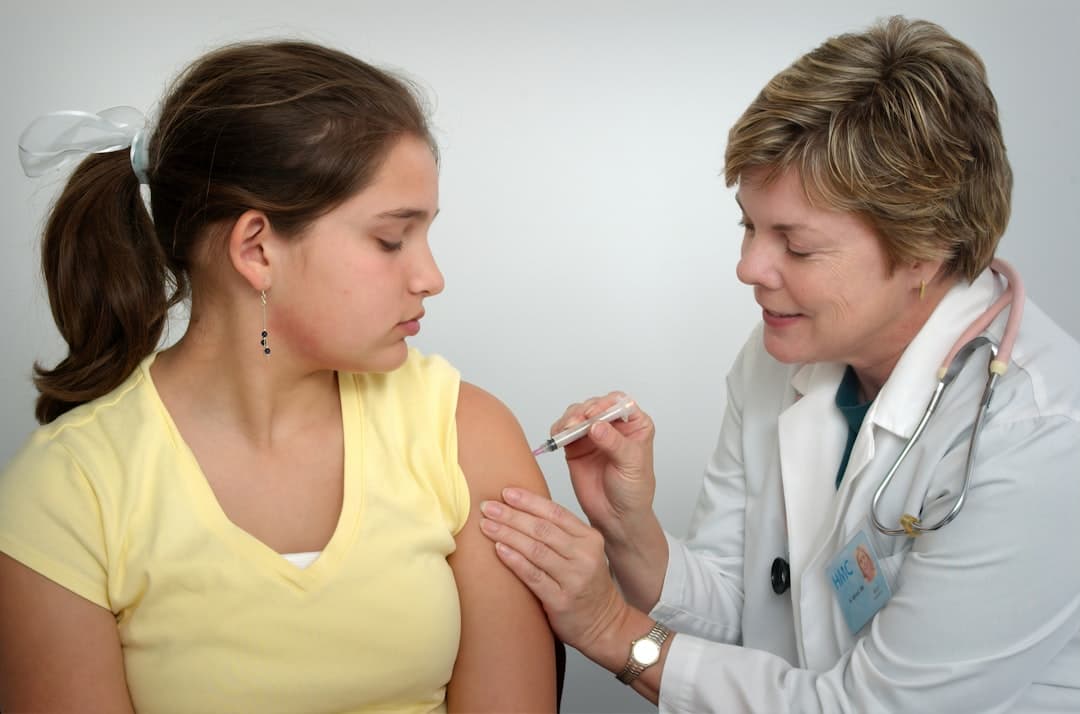
You are sitting in a pediatrician’s office, and the nurse says your baby is due for multiple shots today.
You might trust vaccines in general and still feel your stomach drop.
This is the exact emotional terrain the conversation addresses: it is understandable that parents see 14 diseases, as many as 27 inoculations in the early years, and sometimes five or six shots in one visit, and wonder whether that is too much. The point is not to shame that reaction. The point is to explain it in a way that matches how real-world vaccine decisions are actually made, including the uncomfortable parts.
A key framing runs through everything: safety decisions are not based on “Do we know everything,” they are based on “Do we know enough.” That “enough” is defined as a clear, defensible benefit over risk, especially because vaccines are usually given to healthy people.
This perspective also acknowledges something many people sense but rarely hear stated plainly: modern health information is noisier than ever. The discussion notes a surge in published studies, plus widespread sharing of non peer-reviewed preprints. When the public sees fast-moving science, it can look like experts are changing their minds, when the reality is that the evidence base is still forming.
Important: If you are weighing vaccines for yourself or your child, the most useful next step is usually not more social media. It is a conversation with a clinician who can match the decision to your specific risk factors, timing, and local disease activity.
Innovation always has a human price, vaccines included
The argument here is blunt: every medical innovation has a cost.
Not financial cost. Human cost.
The conversation draws parallels to blood transfusions, chemotherapy, and transplants. Early versions of these therapies could be brutal, because medicine learns by doing, tracking outcomes, and adjusting. The uncomfortable truth is that you cannot fully eliminate uncertainty at the start, because you do not yet have the lived experience of millions of people using the intervention.
Vaccines are different, though, because they are given to healthy people. That raises the bar. A small risk that might be tolerated in chemotherapy can feel unacceptable in vaccination, even if the prevented disease is far more dangerous at a population level.
A practical way the speaker describes decision-making is through gambling metaphors: poker and horse racing. You make the best bet with the information you have, and you accept that doing nothing is also a bet. In infectious disease, “do nothing” can mean allowing predictable hospitalizations and deaths.
This framing can be emotionally hard, but it is also honest. It is one of the video’s unique contributions: it does not pretend uncertainty is a temporary glitch. It treats uncertainty as a permanent feature of real-world medicine.
What an FDA vaccine advisory review actually looks like
Many people imagine a vaccine approval meeting as a quick, political decision.
The described reality is far more procedural and document-heavy.
In the COVID-19 emergency authorizations, the advisory committee members received roughly 150 to 200 pages from the company and another 150 to 200 pages from the FDA reviewing the same data. That is around 400 pages to read for a single meeting, often with about a week to do it.
What those pages represent
They are not a marketing brochure. They are a structured walk through phase 1, phase 2, and phase 3 trials, including the large placebo-controlled trial (for Pfizer, roughly 40,000 participants, and for Moderna, roughly 30,000 participants).
The committee’s job is not to prove perfection. It is to detect major red flags, evaluate whether the trial shows meaningful benefit, and decide whether the known and reasonably foreseeable risks are outweighed by the benefit.
One detail from the discussion shows how cautious this can be: early on, there was worry about a possible signal for Bell palsy (one-sided facial paralysis) in vaccinated groups. The numbers were small, but the signal was taken seriously. Later, after millions of doses, that concern did not hold up as a consistent problem.
That is an important pattern to understand. Early “signals” can vanish when more data arrives, and early reassurance can also be challenged when larger populations reveal rare events.
Did you know? The FDA commonly requires at least about two months of follow-up after the last dose before considering authorization or approval, because historically the most serious vaccine side effects tend to show up within weeks, not years. You can learn more about how vaccine safety is evaluated from the CDC’s vaccine safety overviewTrusted Source.
Rare side effects, the “other shoe,” and why it drops late
If a side effect happens 1 time in 200,000 people, a 30,000-person trial might miss it.
That is not a failure of the trial. It is math.
This section of the conversation is where the “uncomfortable questions” theme becomes most concrete. The speaker describes multiple examples where rare harms only became clear after widespread rollout.
Myocarditis after mRNA vaccines
The discussion describes myocarditis (inflammation of the heart muscle) as occurring primarily in boys and young men, roughly ages 16 to 29, often after the second dose, and often within about 4 days. It is described as generally transient and self-limited, meaning most cases resolved.
The numbers cited in the conversation vary by group. One figure mentioned is roughly 1 in 50,000 overall, with higher rates in the 16 to 29 group, stated as about 1 in 6,600.
This is a key risk-benefit point: even a real side effect can still be considered an acceptable risk if the prevented outcome is far worse and there are not better alternatives.
Clotting after adenovirus-vectored vaccines
The Johnson and Johnson COVID-19 vaccine is discussed as an example where the benefit-risk balance changed because a rare but severe clotting syndrome was identified after widespread use, described as roughly 1 per 200,000 people.
The important nuance is not just that the risk existed. It is that there were other options (mRNA vaccines) available, which changed the ethical calculus.
The post-licensure safety net
A major theme is that vaccines have unusually strong post-licensure monitoring. The discussion highlights linked electronic record systems that can compare outcomes in vaccinated versus unvaccinated groups and detect rare patterns.
For readers who want a concrete example of this kind of monitoring, the CDC describes multiple safety systems, including VAERS and other active monitoring programs, on its vaccine safety systems pageTrusted Source.
What the research shows: Large safety monitoring systems are designed to detect rare side effects that trials cannot reliably capture, and to update recommendations when signals emerge. This is why guidance can evolve even after approval.
“Too many vaccines” and the immune system math parents never see
The fear is intuitive: how can a small baby handle so many shots?
The response is also intuitive once you see the scale of what the immune system does daily.
The discussion makes two complementary arguments.
First, babies are constantly exposed to microbes and antigens. The speaker points out that humans have more bacteria on the surface of the body than human cells, and that everyday exposures like birth, food, and dust are immunologic events.
Second, the “number of vaccines” is not the best measure of immune challenge. What matters is the number and complexity of immune targets inside the vaccines.
A comparison that surprises many people
About 100 years ago, one vaccine many people received was smallpox. Smallpox is described as a large virus with roughly 200 structural and non-structural proteins.
With modern vaccine technology, including recombinant approaches and purified proteins, the total number of immunologic components across today’s routine childhood vaccines is described as lower than what smallpox alone used to present.
That is a counterintuitive idea: more shots, but fewer total immune targets.
This does not mean vaccines are trivial. It means the immune system is built for scale. The discussion uses a striking figure: the body can generate about 10^9 (one billion) new B cells per day, emphasizing that the antigenic “load” of vaccines is a tiny fraction of what the immune system manages routinely.
Pro Tip: If your main worry is “too many at once,” ask your clinician to walk you through which diseases are being prevented at that visit and what the local risk looks like. A calmer decision often comes from replacing a vague fear with a concrete map.
mRNA myths, DNA fragments, and how to judge scary claims
A defining feature of the current era is that misinformation sometimes comes from people with impressive credentials.
That makes it harder for families to know who to trust.
The conversation focuses on a specific example: claims that mRNA vaccines are “contaminated with DNA,” and that this DNA can insert into your genome and cause cancer or autoimmune disease. The speaker’s approach is not “trust me.” It is “here is why that mechanism does not make sense.”
What the mechanism argument is trying to do
The claim suggests a chain of events:
The rebuttal given is that multiple steps in that chain are biologically implausible.
This kind of step-by-step reasoning is the video’s unique communication strategy: it aims to reduce fear by showing where the story breaks.
For readers who want broader context on how mRNA vaccines work and why the mRNA does not stay in the body long-term, the CDC provides a plain-language overview of how mRNA COVID-19 vaccines workTrusted Source.
The “coincidence trap” and emotionally powerful stories
A major point is that humans are compelled by coincidence. If a health event happens after a shot, it can feel caused by the shot.
The discussion includes a painful anecdote: a baby had a seizure while a clinician was preparing a vaccine, later developing epilepsy and dying years later. The point is not that vaccines caused that outcome. The point is that if timing had been slightly different, the family might have been convinced forever that the vaccine caused it, regardless of statistics.
This is why vaccine conversations can become so heated. People are often arguing past each other: one side speaks in population probabilities, the other speaks in personal narrative.
Q: If two doctors disagree about vaccines, how can I decide?
A: Start by asking what kind of evidence each person is using. A biologically plausible mechanism plus consistent real-world data is different from a claim based mainly on temporal coincidence.
Also ask whether the claim matches what is known about how cells handle genetic material. For example, “DNA inserts into your genome from a vaccine” requires several steps that are not easily achieved without specialized viral enzymes.
Dr. Paul Offit, MD (as discussed in the video)
COVID immunity: why you can still get sick and still be protected
One of the most practical insights in the discussion is about expectations.
COVID-19 is framed as a short incubation period, mucosal infection, similar in that sense to influenza and RSV.
That matters because short incubation infections are hard to block at the level of mild illness for long periods.
Long incubation versus short incubation, the expectation reset
This is a core immunology explanation in the conversation:
In this framing, antibodies help prevent mild to moderate disease, but antibodies in circulation decline over months. Memory cells can persist for years, but they may not activate fast enough to prevent symptoms in short incubation infections.
So what is the realistic goal?
Keep people out of the hospital, out of the ICU, and prevent death.
The discussion argues that early in the pandemic, public messaging often failed to explain this clearly, and that overselling protection against any infection set people up to feel lied to when breakthrough infections happened.
Why T cells matter more than most people realize
A repeated theme is that T cells, especially cytotoxic T cells, correlate strongly with protection against severe disease. Antibodies target parts of the spike protein that mutate, but T cell recognition often focuses on more conserved regions.
This helps explain a pattern many people have noticed: even as variants evolved, hospitalization and death rates fell compared to early 2020.
For readers who want general background on immune responses to vaccination and infection, the NIH offers accessible explanations through its educational resources, including immune system basics at NIH MedlinePlusTrusted Source.
Should everyone get a COVID shot every year? A targeted view
The conversation takes a nuanced stance that differs from a universal recommendation.
It argues for prioritizing high-risk groups.
The reasoning is not that vaccination is dangerous for everyone else. It is that for healthy, low-risk people, the benefit may be relatively small and time-limited, making it a “low risk, low reward” choice.
Who is emphasized as higher risk
The discussion highlights groups more likely to be hospitalized or die from COVID-19:
The point is that when vaccine effectiveness against hospitalization is strongest in the months right after vaccination, those months matter most for people with the highest baseline risk.
A concrete effectiveness example from the discussion
The conversation references CDC-presented data suggesting that when the vaccine strain matches the circulating strain, protection against hospitalization can be around 55% for about three months in high-risk groups. When there is a mismatch, the figure cited is around 33% for three months, then waning.
This is presented as a reason to focus efforts where the payoff is highest.
For current official recommendations, readers can check the CDC’s COVID-19 vaccine guidanceTrusted Source, since recommendations can change with variants and seasonality.
»MORE: If you are trying to decide whether a booster makes sense for you, create a one-page “risk profile” to bring to your appointment: age, pregnancy status, immune conditions, major chronic illnesses, and your household exposure risks.
Mandates, backlash, and the quiet role of “busy parents”
Mandates are a values issue, and the conversation treats them as a practical issue too.
In an ideal world, people would be fully informed and choose vaccination without mandates.
But the argument here is that school vaccine mandates have historically prevented outbreaks, and that erosion in mandates and non-medical exemptions can lead to disease resurgence.
The “busy parent” point
One of the most human observations is that mandates do not only address ideological refusal. They also help families who are not opposed to vaccination but are overwhelmed by life: single parents, multiple jobs, limited access to care, missed appointments.
In that sense, mandates can function as a systems-level reminder and access tool, not just a coercive policy.
Measles as a warning signal
The discussion points to rising measles cases as vaccine coverage drops. The CDC tracks measles trends and outbreaks on its measles cases and outbreaks pageTrusted Source.
Measles is used as an example because it is highly contagious and can cause severe outcomes. The conversation cites a rough mortality rate around 0.1% to 0.5%, emphasizing that a return to high case counts could mean preventable child deaths.
Quick Tip: If mandates feel like a blunt tool, focus on the outcome they aim to prevent. Ask, “What level of vaccination keeps outbreaks from reaching infants, pregnant people, and immunocompromised neighbors?” That reframes the issue from politics to protection.
Trust, transparency, and the danger of overselling
Transparency is not the same as flooding people with data.
And persuasion is not the same as marketing.
A major section of the conversation wrestles with whether being fully transparent about uncertainty always increases trust. The example discussed is the 2022 bivalent COVID-19 booster, which was designed to match circulating Omicron variants. Later evidence suggested it was not clearly better than the original formulation, even if it was not worse.
The worry is that if public health leaders overstate “better,” and later evidence shows “not better,” the public concludes, “They do not know what they are doing,” rather than, “Science updated.”
The “truth wrapped in a lie” problem
A particularly useful concept in the discussion is “truth wrapped in a lie.” This is when someone points to a real flaw, like an oversold claim, and then uses it to build a much larger false narrative.
For example, if officials say a product is better when the evidence is uncertain, critics can later say, “They lied,” and then attach unrelated claims about corruption or hidden harms.
This is why the conversation argues for a middle path:
A mostly-bullets section: how to evaluate a vaccine claim in real time
You do not need to become an immunologist to spot weak arguments.
Use this checklist when you hear a scary claim, especially from a credentialed person.
Ask what would have to be true biologically for the claim to work. If someone says DNA from a vaccine inserts into your genome, ask what steps would be required (cell entry, nuclear entry, integration enzymes). If the person cannot explain the steps, that is a red flag.
Separate “after” from “because of.” Many health events happen every day in a population. A symptom occurring after vaccination can be coincidence unless rates are higher in vaccinated groups than in comparable unvaccinated groups.
Look for active surveillance confirmation. Rare side effects that are real often show up in large monitoring systems. The faster a claim spreads, the more important it is to see whether systems like those described by the CDCTrusted Source detect a signal.
Check whether the claim explains both sides of the ledger. Good risk communication includes what the vaccine prevents (hospitalization, death, complications) and what it might cause (rare adverse events), with numbers when possible.
Notice emotional manipulation. If the message relies mainly on outrage, identity, or “they are hiding it,” rather than mechanisms and comparative rates, it may be designed to persuade rather than inform.
A calmer decision often comes from slowing the information down.
Key Takeaways
Frequently Asked Questions
- How can vaccines be called safe if rare side effects exist?
- “Safe” in medicine usually means benefits clearly outweigh risks, not that risks are zero. Rare side effects may only appear after millions of doses, which is why ongoing safety monitoring is a key part of vaccination programs.
- Is it possible for DNA fragments in vaccines to alter your DNA?
- The claim requires multiple difficult biological steps, including reaching the nucleus and integrating into the genome without specialized enzymes. Current evidence and basic cell biology make this scenario unlikely, but discuss personal concerns with a clinician.
- Why do people still get COVID after vaccination?
- COVID-19 is described as a short incubation respiratory infection, so protection against mild illness can fade as antibodies decline. Vaccination can still reduce the risk of severe outcomes like hospitalization and death, especially in higher-risk groups.
- Are childhood vaccines “too much” for a baby’s immune system?
- Babies encounter many antigens daily through normal life, and modern vaccines often contain fewer immune targets than older vaccines like smallpox did. If you are worried, ask your pediatric clinician to explain the schedule and disease risks in your area.
- Do vaccine mandates help people who are not anti-vaccine?
- They can, because some families miss vaccines due to access barriers, time constraints, or disrupted care rather than ideological refusal. Mandates can function as a system-level prompt that improves overall coverage.
Get Evidence-Based Health Tips
Join readers getting weekly insights on health, nutrition, and wellness. No spam, ever.
No spam. Unsubscribe anytime.