Lower Resting Heart Rate for Better Sleep Quality
Summary
A striking claim in the video is that the strongest predictor of nighttime sleep quality is resting heart rate, and that “everything” is aimed at lowering beats per minute. The speaker links a lower resting heart rate with falling asleep in 1 to 3 minutes, averaging over 2 hours of REM and 2 hours of deep sleep, and being awake less than 30 minutes per night. This article investigates that viewpoint, explains why heart signals like resting heart rate and *heart rate variability* may track recovery, and offers practical, non-prescriptive ways to experiment safely. If you have heart symptoms or take heart-related medications, involve a clinician.
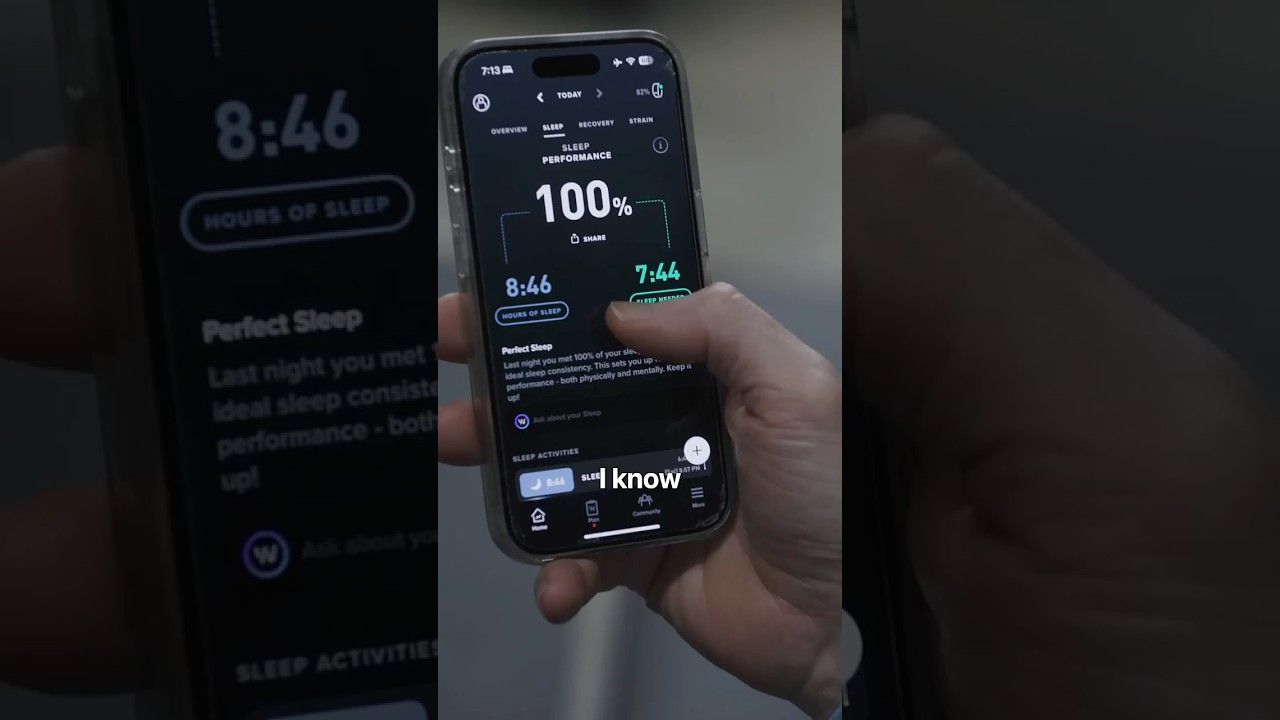
The speaker ties “the best sleep score in human history” to one metric.
This perspective argues it is the single strongest predictor of nighttime Sleep Quality, and that lowering beats per minute is the lever that moves everything else.
The video’s bold claim: resting heart rate predicts sleep
The story is unusually specific. A lower resting heart rate is framed as the reason the speaker’s head hits the pillow at 8:30 and sleep happens in 1 to 3 minutes.
Then come the markers used to define “exceptional sleep”: over 2 hours of REM, 2 hours of deep sleep, and being awake less than 30 minutes per night. The video’s unique angle is not “sleep hygiene” first. It is a heart-first strategy where sleep is treated as the downstream result.
Pro Tip: If you want to explore this approach, pick one primary metric to watch for 2 weeks, such as nightly resting heart rate, and avoid changing five habits at once.
Why a lower heart rate might track better sleep
A lower resting heart rate at night can be a sign that the body is shifting into a calmer, recovery-oriented state, often associated with more parasympathetic activity. That does not guarantee perfect sleep, but it can be a useful clue.
What’s interesting is that resting heart rate rarely acts alone. It tends to move alongside heart rate variability (HRV), another signal commonly used to estimate recovery and stress balance. Research looking at relationships between resting heart rate, HRV, and related factors suggests these measures can be meaningfully connected in real-world physiology, including how the body responds to strain and recovery cycles (resting heart rate and HRV relationshipsTrusted Source).
Did you know? Many wearables estimate sleep stages using movement plus heart signals, so changes in resting heart rate can sometimes shift how “REM” and “deep” are scored, not just how you feel.
How to test this idea in real life (without guessing)
This is where the video’s viewpoint becomes practical: treat resting heart rate like a nightly “thermometer” for how revved up you are.
A simple 7-night experiment
Lock in a consistent lights-out time. The video uses 8:30 as the anchor. Choose a time you can repeat, because irregular timing can keep your body on alert.
Track two outcomes, not ten. Record (a) resting heart rate during sleep and (b) one sleep outcome you care about, such as minutes to fall asleep or time awake at night. If you use a wearable, keep the device and settings the same all week.
Add one calming lever at a time. For example, try a 10 to 15 minute wind-down routine, then see whether your heart rate trend changes over several nights.
Lifestyle levers that may lower nighttime heart rate
What the research shows: Heart-related signals like resting heart rate and HRV often move with stress and recovery patterns, which is one reason they can be useful to monitor alongside sleep (resting heart rate and HRV relationshipsTrusted Source).
When to be cautious, and when to ask for help
Chasing a lower resting heart rate is not always benign. A “low” number can be normal for athletes, but a sudden change, symptoms, or medication effects deserve medical input.
Important: If you have chest pain, fainting, new palpitations, shortness of breath at night, or a resting heart rate that is unusually high or suddenly different for you, consult a clinician promptly. If you take beta-blockers, thyroid medication, or stimulants, ask your prescriber before making major sleep or exercise changes.
Q: If I fall asleep in 1 to 3 minutes, is that always a good sign?
A: Not necessarily. Very fast sleep onset can happen with excellent sleep readiness, but it can also reflect sleep deprivation or an irregular schedule. If you are falling asleep instantly yet still feel unrefreshed, it is worth reviewing total sleep time, sleep timing, and possible sleep disorders with a health professional.
Health educator, MPH
Key Takeaways
Sources & References
Frequently Asked Questions
- What is a good resting heart rate during sleep?
- It varies by age, fitness, medications, and health conditions, so there is not one perfect number for everyone. A more useful approach is tracking your personal baseline and watching for sustained changes or symptoms, then discussing concerns with a clinician.
- Can improving sleep lower resting heart rate, not just the other way around?
- Yes, the relationship can be bidirectional. More consistent, restorative sleep may reduce stress load and support recovery, which can nudge resting heart rate downward over time.
- Do wearables accurately measure REM and deep sleep?
- Wearables can be helpful for trends, but their sleep stage estimates are not the same as clinical sleep testing. Use the stage numbers as rough signals, and prioritize how you feel and function during the day.
Get Evidence-Based Health Tips
Join readers getting weekly insights on health, nutrition, and wellness. No spam, ever.
No spam. Unsubscribe anytime.