The LDL Paradox: When “Normal” LDL Still Fails
Summary
A striking 2009 analysis of more than 136,000 coronary artery disease hospitalizations found that nearly half of patients arrived with LDL cholesterol under 100 mg/dL. This video uses that “LDL paradox” to ask a different question: if LDL is often “normal,” what else is driving plaque and heart events? The discussion centers on immune activation, oxidized or modified LDL, and leaky, dysfunctional endothelium that may allow lipoproteins into the artery wall. It also highlights real-world clues like erectile dysfunction, insulin resistance, and lack of exercise, plus practical ways to think beyond LDL alone.
🎯 Key Takeaways
- ✓A large 2009 cohort found many hospitalized coronary patients had LDL under 100 mg/dL, raising questions about what else contributes to events.
- ✓This perspective emphasizes *immune activation* and *modified or oxidized LDL* as key triggers for plaque inflammation, not LDL concentration alone.
- ✓Endothelial dysfunction (a “leaky” vessel lining) may help explain how lipoproteins enter the artery wall, especially with smoking, high blood sugar, high blood pressure, and inactivity.
- ✓Low HDL (often under 40 mg/dL in the cohort) is framed as a strong clue of poor metabolic health and higher risk, even when LDL is not high.
- ✓Exercise and outdoor light exposure are positioned as practical anti-inflammatory tools that may improve vascular health beyond what a lipid panel shows.
A clinician opens the discussion with a paper he calls “the elephant in the room.”
It is not a fringe preprint or a conspiracy blog. It is a large, mainstream analysis of people hospitalized for coronary artery disease, the moment where chest pain, shortness of breath, unstable symptoms, or a heart attack brings someone to the hospital.
And the question he wants you to sit with is uncomfortably simple: What were their LDL cholesterol levels at admission?
The “elephant in the room”: low LDL at the hospital
The headline result that drives the entire video is this: in a large 2009 cohort of coronary artery disease hospitalizations, almost half of patients had LDL cholesterol below 100 mg/dL on admission.
That matters because many people are taught a straightforward story: LDL is the “bad cholesterol,” lower is better, and if you keep LDL under common targets, you are safe. This video argues the real world is messier.
One more detail sharpens the point. The discussion notes that more than half of these hospitalized patients also had HDL cholesterol below 40 mg/dL, and it frames low HDL as a stronger signal of poor metabolic health than high LDL in many cases.
Did you know? In this 2009 analysis of roughly 136,000 coronary artery disease hospitalizations, nearly half of patients arrived with LDL under 100 mg/dL, a level many clinicians consider “at goal.”
This does not mean LDL is irrelevant. It means that LDL, by itself, may not fully explain who ends up with plaque, rupture, or a hospitalization.
What the 2009 paper actually found, and what it did not
The video’s investigative move is to separate two things that often get blended together online: what a study shows, and what we assume it means.
The LDL target story runs into a paradox
The “continual exposure hypothesis” is described as a dominant idea in cardiovascular prevention. The longer you are exposed to higher levels of apoB-containing lipoproteins (LDL, VLDL, remnant particles), the higher the chance those particles contribute to atherosclerosis.
So when a large cohort shows many hospitalized patients already had LDL under 100 mg/dL, one reaction is to say: “Then we should push LDL even lower.” The paper itself is characterized as supporting lower LDL goals and exploring ways to raise HDL.
But the video challenges what gets ignored when the conclusion becomes “lower must be better.”
The missing variable: why is the immune system activated?
The argument is that plaque is not just a passive “fat clog.” It is an inflammatory, immune-involved process. If you focus only on LDL concentration, you may miss why LDL becomes dangerous in the first place.
This is where the discussion widens to mechanisms: LDL oxidation or modification, immune cell recruitment, and endothelial dysfunction.
What the research shows: Some cardiovascular literature discusses “cholesterol paradox” patterns in certain conditions, where lower cholesterol associates with worse outcomes, likely reflecting illness severity, inflammation, or frailty rather than protection. See an example discussion in atrial fibrillation populations: Cholesterol paradox in atrial fibrillationTrusted Source.
A key caution, though, is that paradox findings do not automatically mean LDL does not matter. They often mean that context matters, including acute illness, chronic disease, inflammation, nutrition status, and medication use.
Atherosclerosis as an immune problem, not just a lipid problem
The core “unique perspective” of this video is a reframing: think about atherosclerosis through the lens of autoimmunity.
That is a strong claim, and the video treats it as a working model rather than a settled verdict. The point is not that heart disease is identical to lupus or rheumatoid arthritis. The point is that plaque behaves like a chronic immune-inflammatory process, with both innate and adaptive immune responses involved.
The foam cell story, slowed down
Here is the sequence the discussion emphasizes, in plain language.
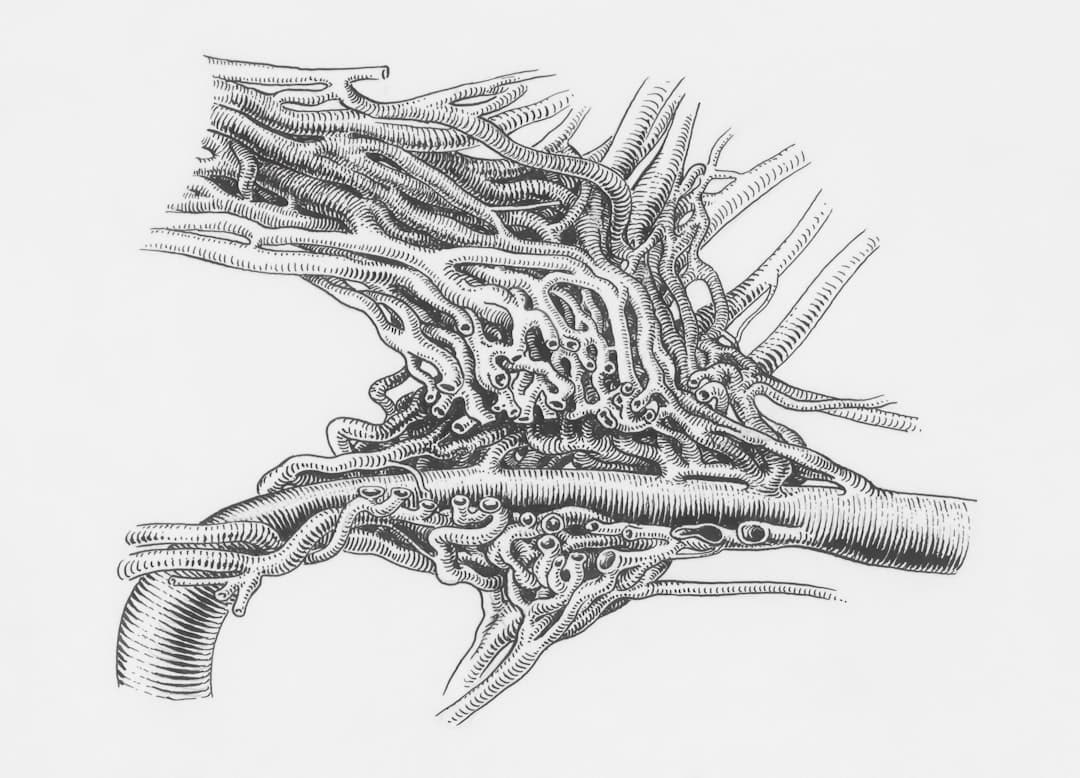
LDL particles circulate in blood. Under certain conditions, LDL can become oxidized or otherwise modified near the vessel wall. When that happens, immune cells called monocytes are recruited, enter tissue, and transform into macrophages. Macrophages take up modified LDL through receptors that “scavenge” these particles.
As macrophages fill with lipid, they become foam cells, an early building block of the fatty streak that can evolve into plaque.
What makes this framing different is the emphasis on the trigger: immune activation.
The video quotes a paper describing how LDL accumulates in the arterial intima, becomes modified by oxidation and or aggregation, and then acts as a chronic stimulator of immune responses, with the idea that atherosclerosis can be likened to an autoimmune disease.
Why this matters for everyday people
This immune-first framing changes the practical questions.
Instead of only asking, “How do I lower LDL?” you also ask:
The video also notes an important clinical reality: many inflammatory markers can look “normal” for a long time. C-reactive protein (CRP) may not rise dramatically until disease processes have been present for years, and it can spike briefly during infections (like flu or COVID) and then return to baseline.
How does LDL get into the artery wall? The endothelium angle
The discussion pivots to a question that is often skipped in casual cholesterol talk: how do large lipoprotein particles cross into the vessel wall at all?
In healthy tissue, the endothelium (the inner lining of blood vessels) functions as a selective barrier. Lipoproteins are large macromolecules, and they do not simply drift through intact cells.
So what changes?
Endothelial dysfunction and “leakiness”
A key mechanism highlighted is endothelial dysfunction, sometimes described as a “leaky” or impaired vessel lining. The video links this to common, real-world exposures and conditions:
This framing suggests that lipids and the vessel wall are not separate stories. The state of the endothelium may influence whether lipoproteins can enter the arterial wall and participate in plaque biology.
The video references the concept of endothelial transcytosis (a process by which cells transport particles across themselves), positioning it as a modern mechanistic lens on atherosclerosis.
A practical measurement that is not mainstream yet
The discussion mentions arterial pulse wave velocity as one way to assess arterial stiffness and vascular elasticity, and notes it is not routinely accessible in mainstream care for many patients.
The point is not that everyone needs this test. It is that vascular function is measurable, and it may add context beyond a standard lipid panel.
Pro Tip: If you are tracking cardiovascular risk, consider asking whether your clinician can evaluate vascular health beyond cholesterol numbers, for example blood pressure trends, glucose control, and in some settings arterial stiffness measures.
Real-world clues: ED, insulin resistance, and “normal” labs
A theme running through the video is that cardiovascular risk often shows up as everyday clues before it shows up as a dramatic lab abnormality.
Erectile dysfunction as a vascular signal
A punchy line from the video is that ED can hint at another ED: endothelial dysfunction.
Erectile function depends on healthy blood flow and responsive blood vessels. If small vessels are impaired, symptoms may appear there before larger vessels cause chest pain.
This is not a diagnosis, and ED has multiple causes, including medications, stress, and hormonal factors. But the video argues it is a symptom worth taking seriously as a potential vascular warning sign, especially alongside other risk factors.
For women: look for metabolic context
The video acknowledges that women do not have the same “ED clue,” and instead points to a cluster of indicators that may suggest endothelial dysfunction or metabolic strain:
This is a pattern-based approach. One factor alone does not equal disease, but multiple factors together can raise suspicion that vascular function deserves attention.
The athlete examples: LDL can rise when health is excellent
One of the most distinctive parts of the video is the use of athlete lab examples to complicate simplistic LDL fear.
The discussion shows an elite athlete whose LDL reportedly rose to well over 350 mg/dL after a fasted exercise session. Another endurance athlete running about six miles daily showed elevated LDL in a post-exercise window.
The argument is not that extremely high LDL is always harmless. It is that LDL values can be context-dependent, and a single snapshot may not capture risk without the surrounding picture: blood pressure, insulin sensitivity, inflammation, fitness, and vascular function.
Important: If you ever see very high LDL values (for example, above 190 mg/dL, and especially values in the 300s), do not assume it is “just exercise.” It is worth repeating the test under standardized conditions and discussing secondary causes and family history with a clinician.
Practical next steps: a broader risk conversation to have
This video does not tell viewers to ignore LDL. It argues for expanding the checklist.
Here are practical, video-aligned ways to apply the “LDL paradox” idea without overcorrecting.
1) Reframe the goal from “LDL only” to “vascular environment”
The discussion repeatedly returns to the vessel wall and immune activation.
If the endothelium is healthy and inflammation is low, the argument goes, the same LDL number may not carry the same meaning as it would in someone with insulin resistance, smoking exposure, high blood pressure, or chronic inflammatory disease.
2) Consider inflammation and oxidation context (with your clinician)
The video mentions specialized testing that may look at oxidized LDL and inflammatory markers. It also notes the interpretive challenge: inflammation can be subtle for years, and acute infections can temporarily spike markers like CRP.
A practical approach to discuss with a clinician might include:
3) Take autoimmune and inflammatory conditions seriously
Another distinctive claim is that people with autoimmune diseases tend to have higher cardiovascular risk and faster plaque progression. The video lists multiple sclerosis, rheumatoid arthritis, lupus, asthma, allergies, and more.
This aligns with broader clinical awareness that chronic inflammatory conditions can increase cardiovascular risk. It also supports the video’s central thesis: you cannot fully disentangle LDL from the immune system.
Expert Q&A
Q: If my LDL is under 100 mg/dL, does that mean I am protected from heart disease?
A: Not necessarily. This video highlights that many hospitalized coronary artery disease patients had LDL under 100 mg/dL, suggesting other factors like endothelial dysfunction, insulin resistance, and inflammation may still drive risk.
LDL is still one piece of the puzzle, but it is best interpreted alongside blood pressure, glucose control, smoking history, family history, and inflammatory or autoimmune conditions.
Health education summary based on the video’s clinical framing
4) Lifestyle levers emphasized in the video (with real-world details)
The closing portion of the transcript shifts from mechanisms to daily life. Two themes stand out: exercise and light exposure.
This is not presented as a cure. It is presented as a way to lower chronic inflammation and improve metabolic and endothelial health.
Exercise as an anti-inflammatory signal
The video describes exercise as producing “exerkines” (exercise-induced signaling molecules) that may have anti-inflammatory effects and are associated with lower risk of cardiovascular disease, autoimmune disease, and all-cause mortality.
It also includes a viewer comment about losing fitness after moving from a sunny place to a low-sun environment, and a direct nudge to restart exercise even when circumstances change.
Light, outdoors time, and vitamin D nuance
The video argues that supplements can help if you are deficient, but they cannot fully replace sunlight and outdoor exposure. It suggests using a lux meter and aiming for about 10,000 lux around the middle of the day, even on cloudy days, as a practical target for “getting outside.”
That is a lifestyle metric, not a medical prescription. Still, it is a concrete example of the video’s style: measure the environment, not just the blood.
»MORE: If you want to make this actionable, create a 2-week “vascular habits” log: daily steps, two strength sessions per week, blood pressure readings (if you track them), and 10 to 30 minutes of outdoor light exposure midday when possible.
5) Medication questions raised, without easy answers
The transcript also raises a thoughtful question about statins: are benefits more related to LDL lowering, anti-inflammatory effects, or both?
This is not settled in the video, and it should not be settled casually. If you take a statin or are considering one, the safest move is to discuss your full risk profile with your clinician, including family history and any autoimmune or inflammatory conditions.
What the research shows: Cardiovascular events can worsen vulnerability and functional decline in older adults, connecting heart events to frailty trajectories. See: The Aggravation of Frailty by Cardiovascular EventsTrusted Source.
Key Takeaways
Sources & References
Frequently Asked Questions
- Why would someone have a heart attack if their LDL is under 100 mg/dL?
- This video argues that LDL is only one variable. Endothelial dysfunction, insulin resistance, smoking history, and immune-driven inflammation (including oxidized or modified LDL) may still promote plaque and trigger events.
- Is low HDL more important than high LDL?
- The video frames low HDL (often under 40 mg/dL) as a strong clue of poor metabolic health. In practice, clinicians usually interpret HDL alongside triglycerides, glucose markers, blood pressure, and overall risk.
- What is endothelial dysfunction, in simple terms?
- It means the inner lining of blood vessels is not working normally. The video links it to factors like smoking, high blood sugar, high blood pressure, and inactivity, and suggests it may make it easier for lipoproteins to enter the vessel wall.
- Can exercise temporarily raise LDL cholesterol?
- The video shows examples where LDL rose after fasted exercise or in endurance athletes. If you see unexpected spikes, it is reasonable to repeat testing under standardized conditions and review the results with a clinician.
- Do statins reduce risk mainly by lowering LDL or by reducing inflammation?
- The video raises this as an open question and notes statins have anti-inflammatory properties in addition to LDL lowering. If you are considering medication changes, it is best to discuss benefits and risks with your prescribing clinician.
Get Evidence-Based Health Tips
Join readers getting weekly insights on health, nutrition, and wellness. No spam, ever.
No spam. Unsubscribe anytime.